
A virtual teammate for every task.

Instant answers for providers. Real savings for your team.
Expand automation into other critical workflows.
Coordination of Benefits
Automate outbound voice calls to collect and verify additional coverage details, reducing manual follow-ups and accelerating accurate claims processing.
Accident Claim Coordination
Trigger AI-driven outbound calls to gather required accident details from members and automatically route structured data into your claims workflow.
Prior Authorization
Give providers and members real-time prior authorization status through AI-assisted checks—cutting call volume and easing administrative strain.
Member Benefit Navigation
Extend AI-guided benefit support beyond the app with voice and SMS, meeting members where they are with consistent, plan-aware guidance.
Efficiency for teams. Clarity for providers. Ease for members.
Automate the routine. Elevate the service.
- Reduce call center volume and increase first-contact resolution
- Monitor and record all conversations, and call logs for audit ready compliance
- Trigger escalations to UM teams only when needed
- Mirror workflows across chat, voice, and portal—one record, no repetition
- Tracking for record keeping and audit support

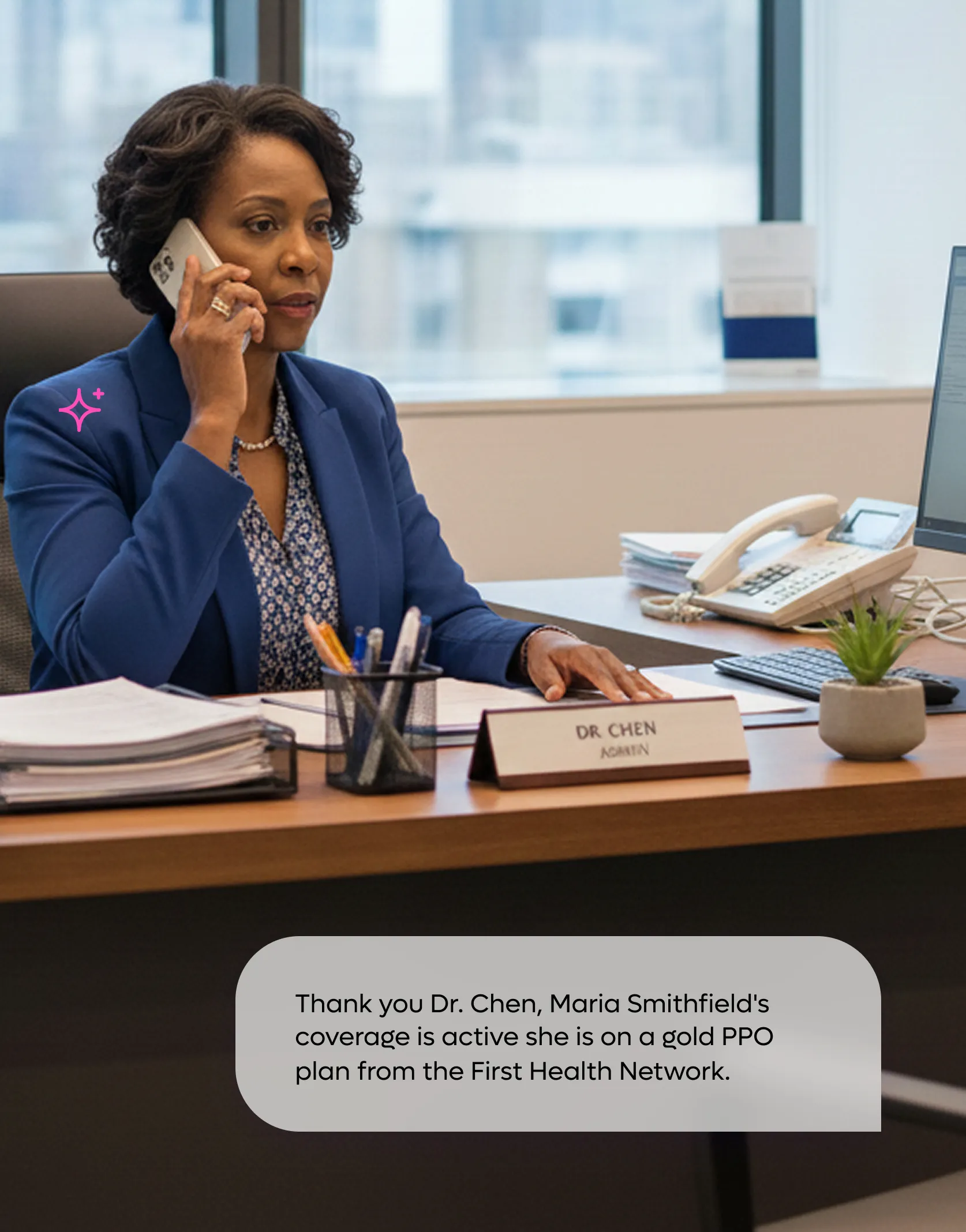
Faster access to the answers they need
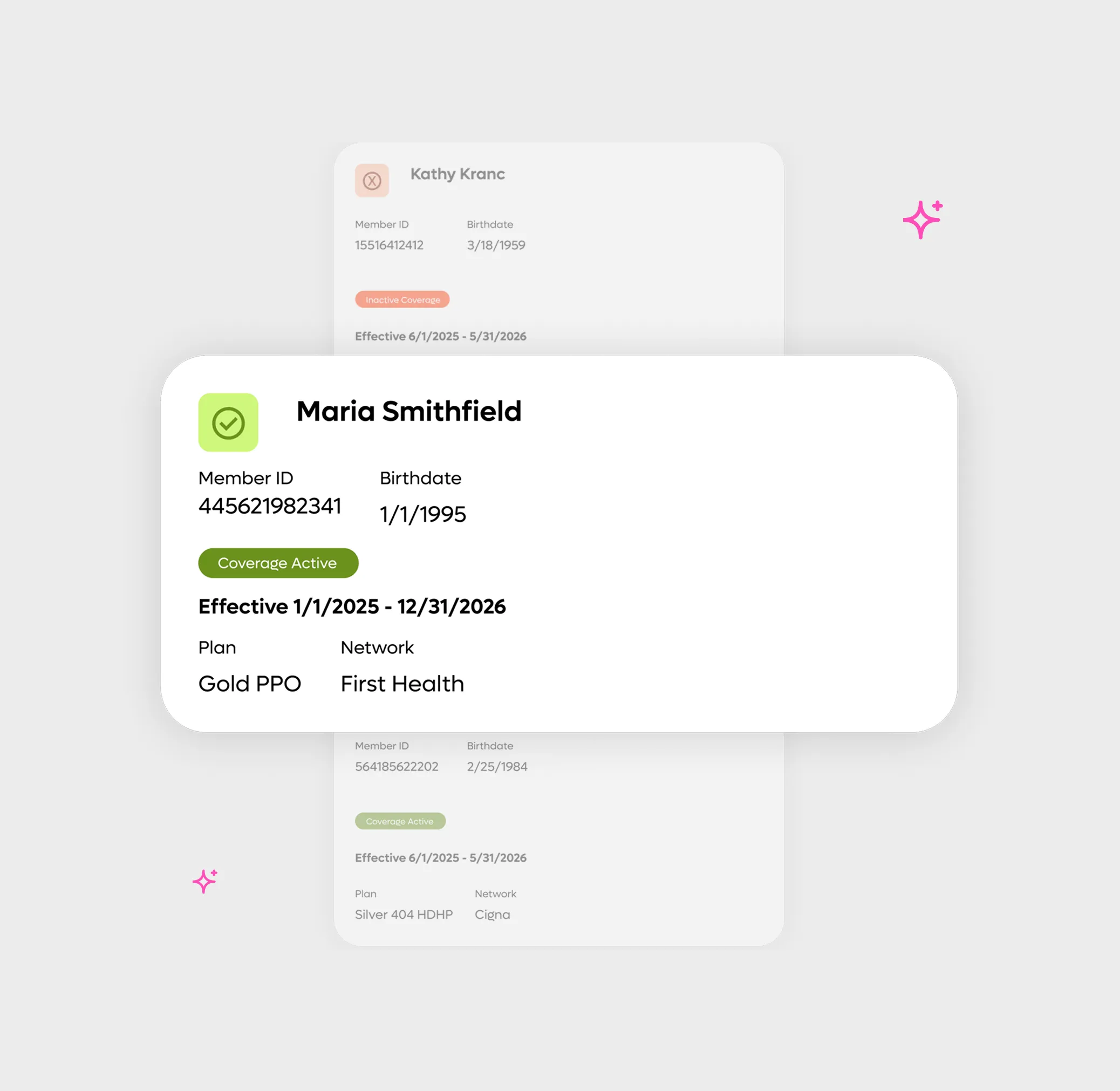
- 24/7 voice and chat support for eligibility and claims
- Seamless submission and status tracking
- Fewer inbound calls to your service team
- Real-time data access with fewer delays or errors
No more hold music
- AI agents trained on plans, documents, and benefits
- Speak in your language—Opyn answers in yours
- Faster issue resolution and less frustration
- Optional escalation to live help when needed
- Tech support agent available for account or login help

Works with the systems you already use.
Opyn’s AI agents integrate directly into your existing engagement platforms and workflows—no replacement, rebuild or migration required. Use the agents on their own or connect them into the full Opyn platform whenever you're ready.






