Streamline what sits between your claims system and your members.


Reduce demand. Lower costs. Strengthen your service.
- Reduce call-center burden
- Lower OpEx
- Faster resolutions at scale
- Enterprise-grade stickiness
- Stronger compliance alignment
Opyn AI features that power every touchpoint.
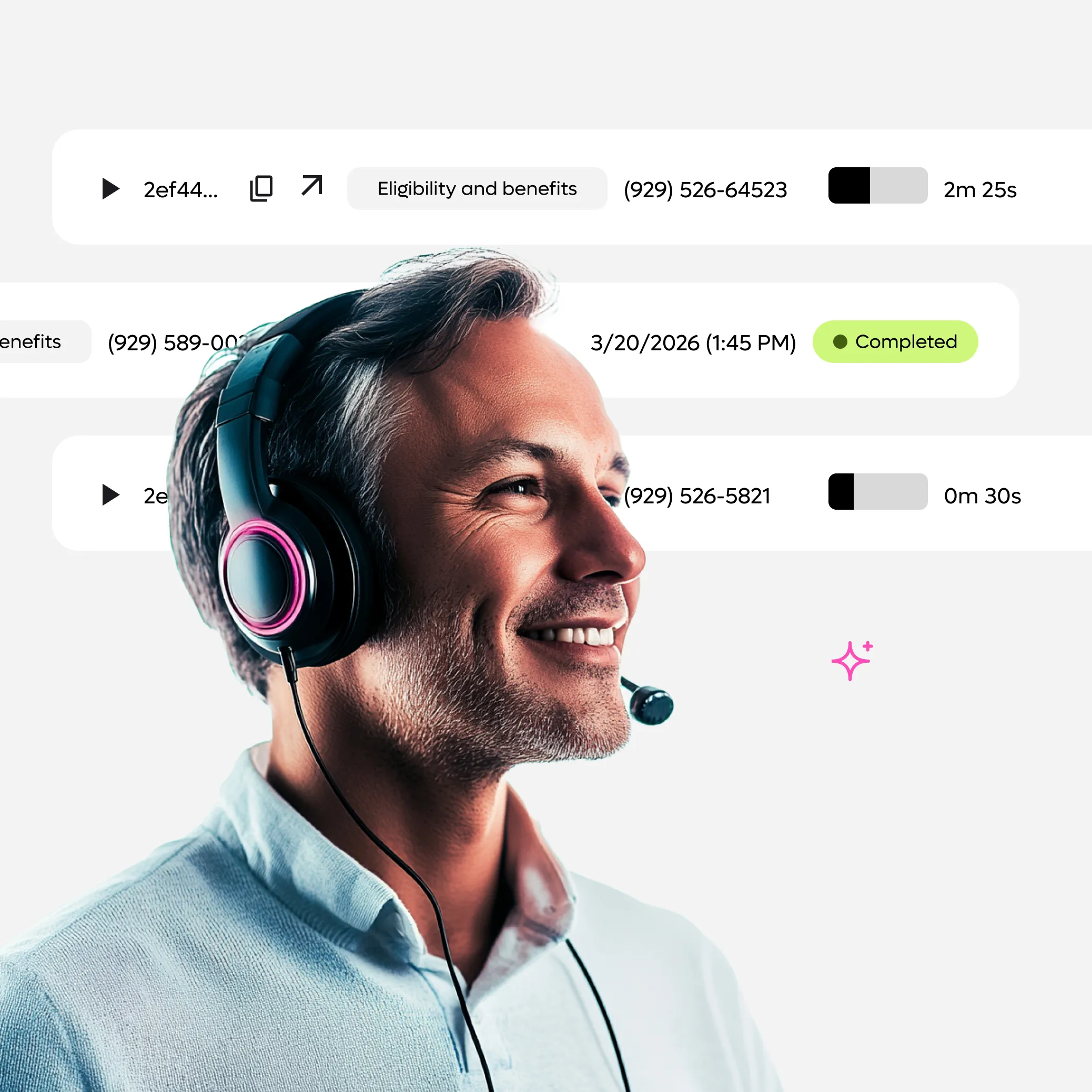
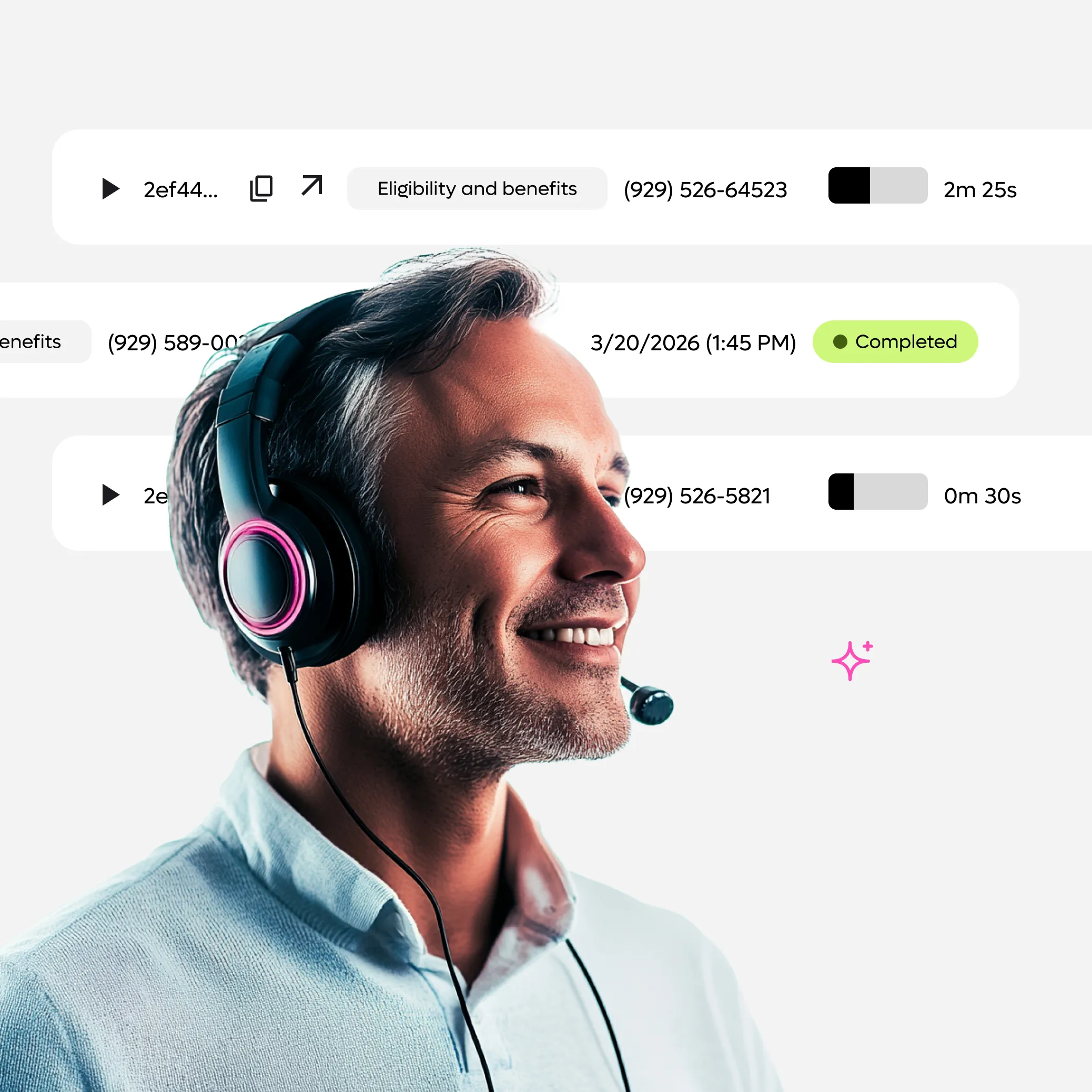
Your Virtual Front Line for Provider Calls
Providers aren’t your customers—but they account for a disproportionate share of your call volume. Our AI-Powered Provider Interaction Agent handles their most common questions, instantly.
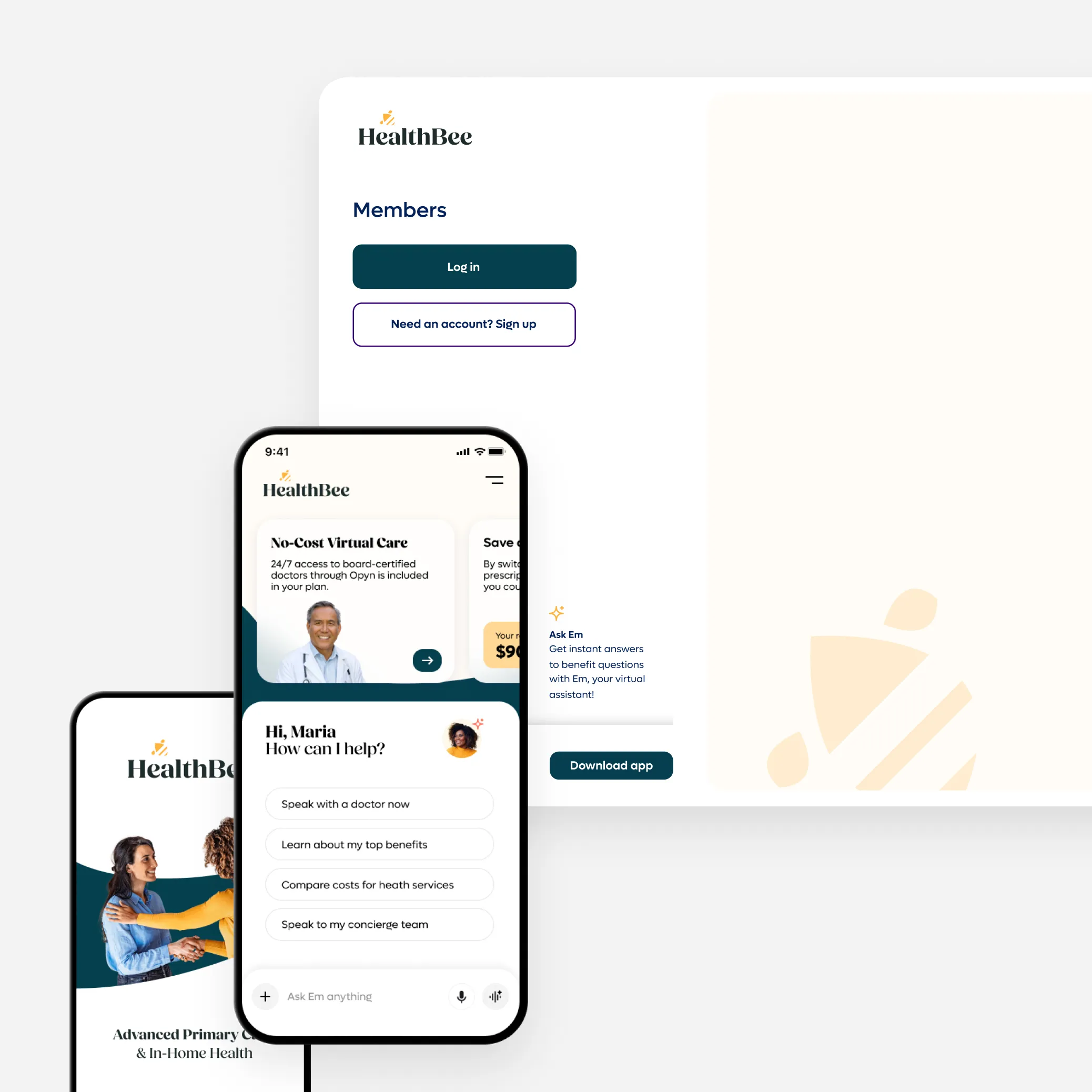
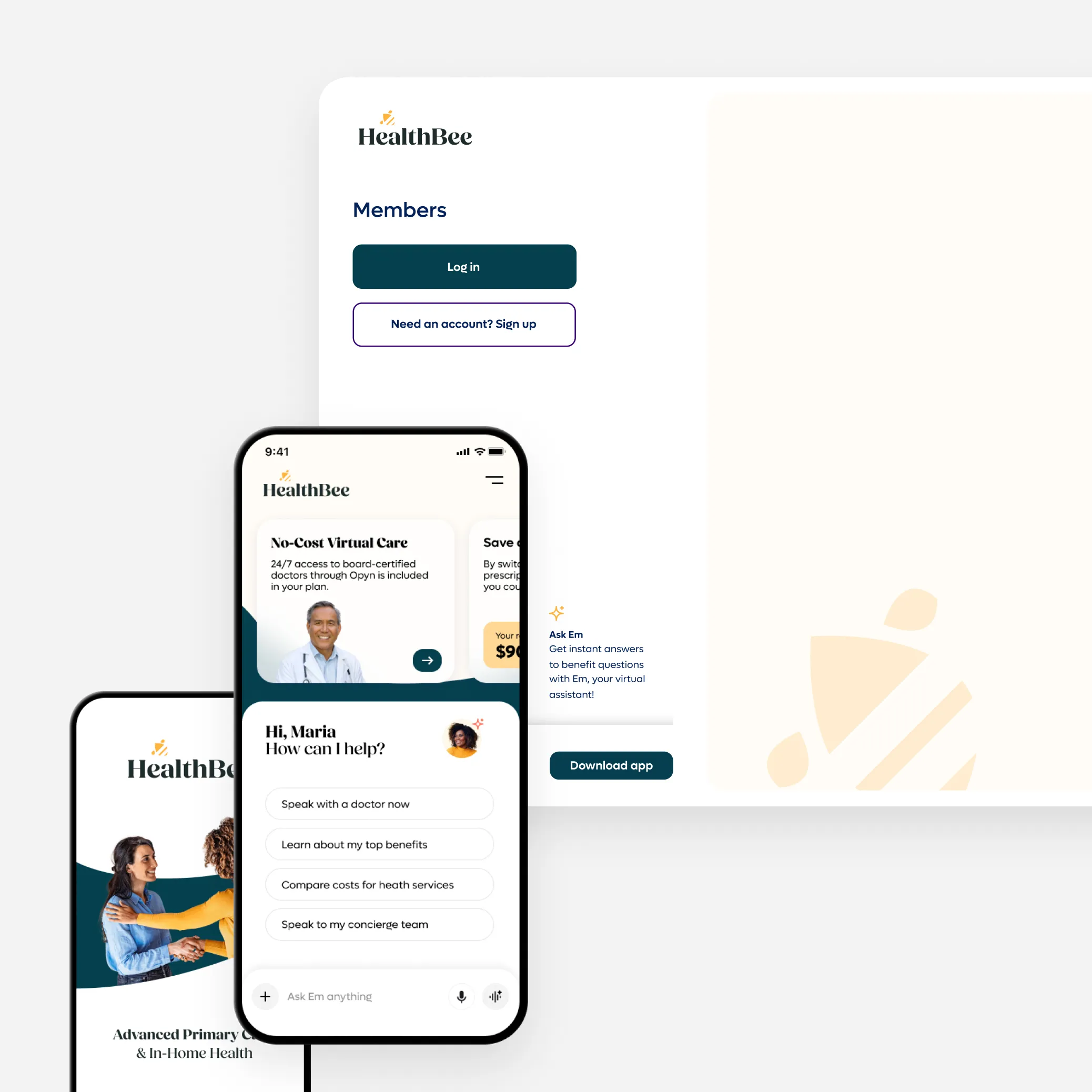
Own the Experience, AI the Navigation
Provide a unified, white-label platform that connects members, employers and brokers under your brand. Our AI assistant helps members self-navigate their health plans in real-time, reducing your administrative load by turning complex back-office workflows into seamless, automated experiences.
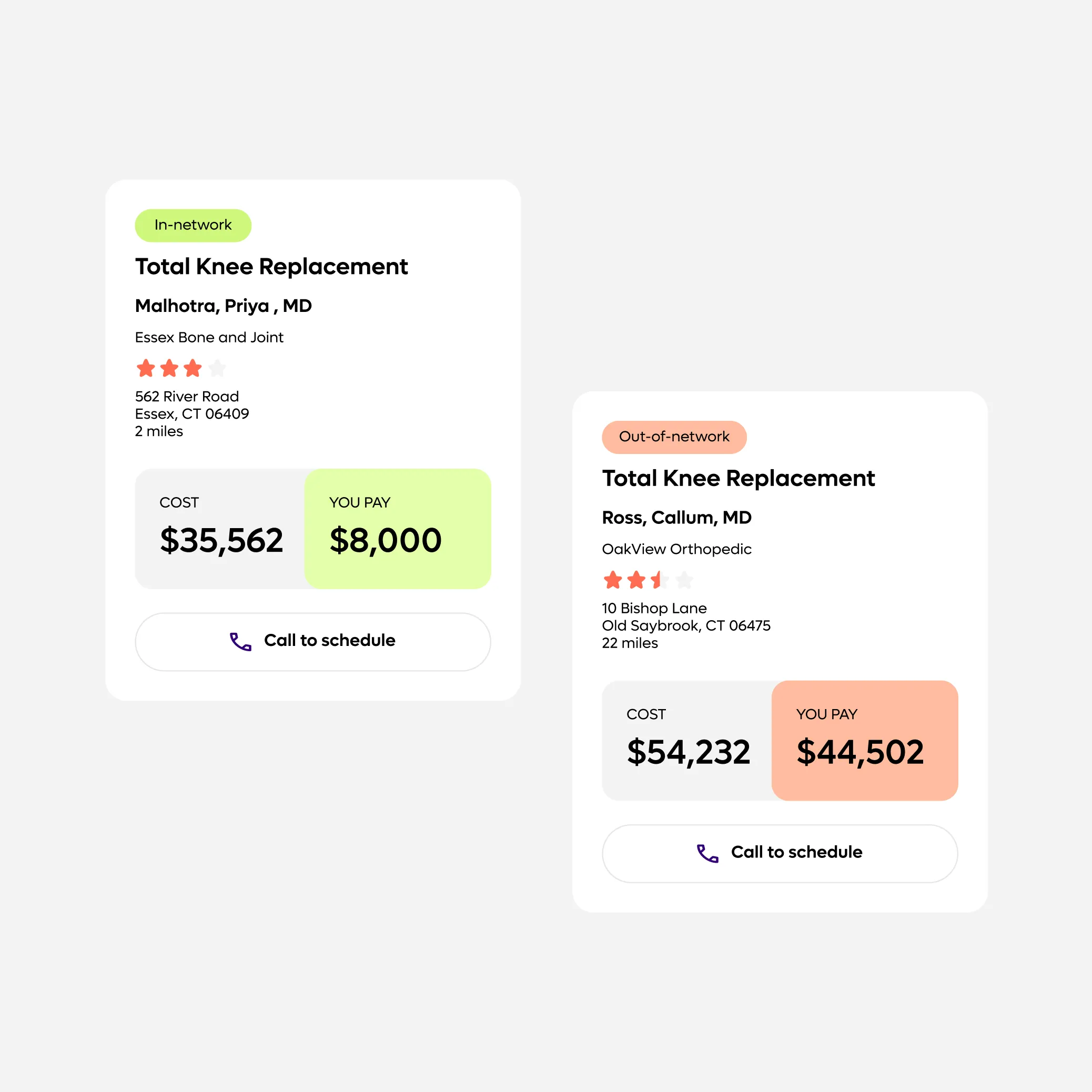
Compliance Turned Active Guidance
Turn Transparency in Coverage from requirement to real member guidance. Our TiC Solution interprets pricing data through AI assistance, proactively guiding members toward low-cost, high-quality providers and services.
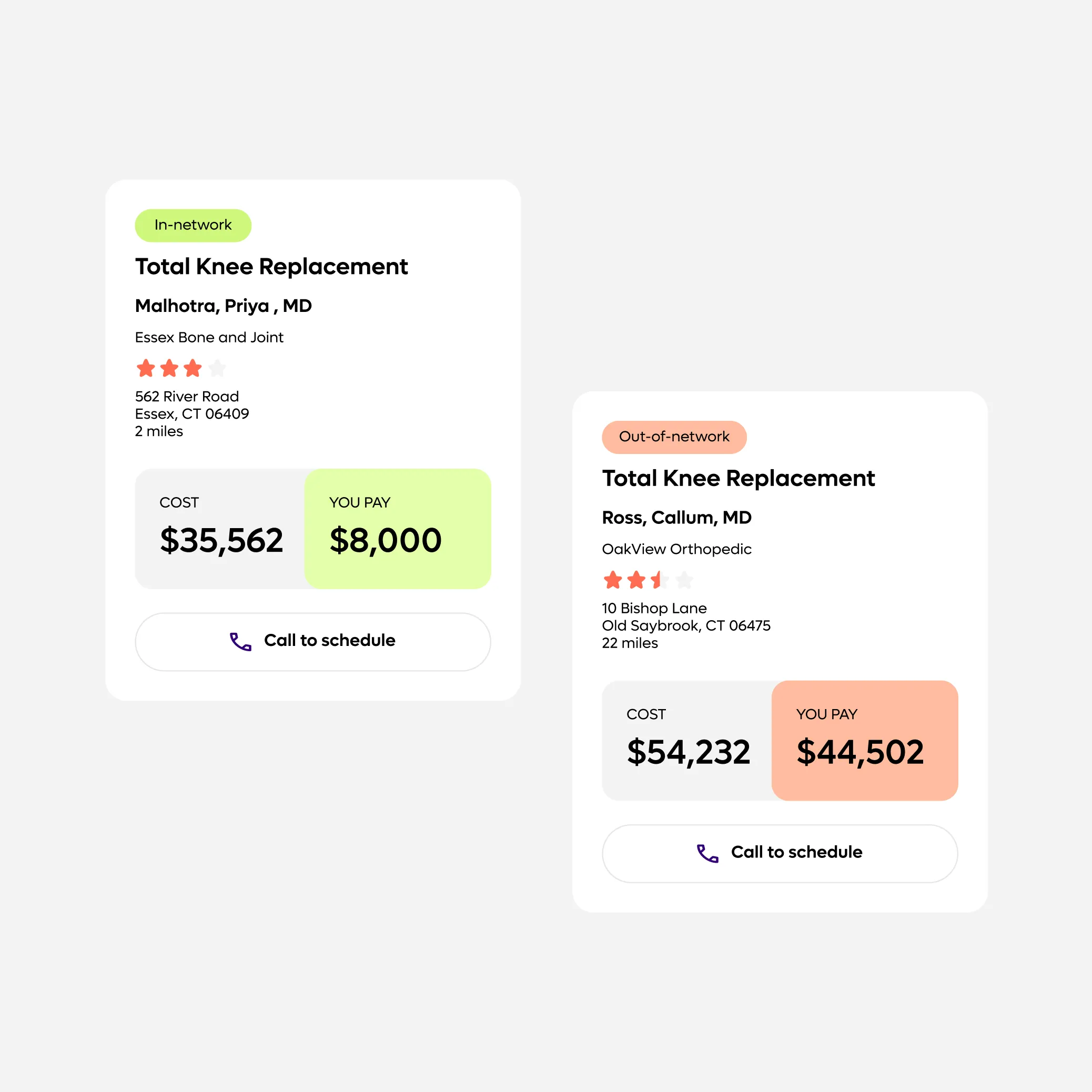
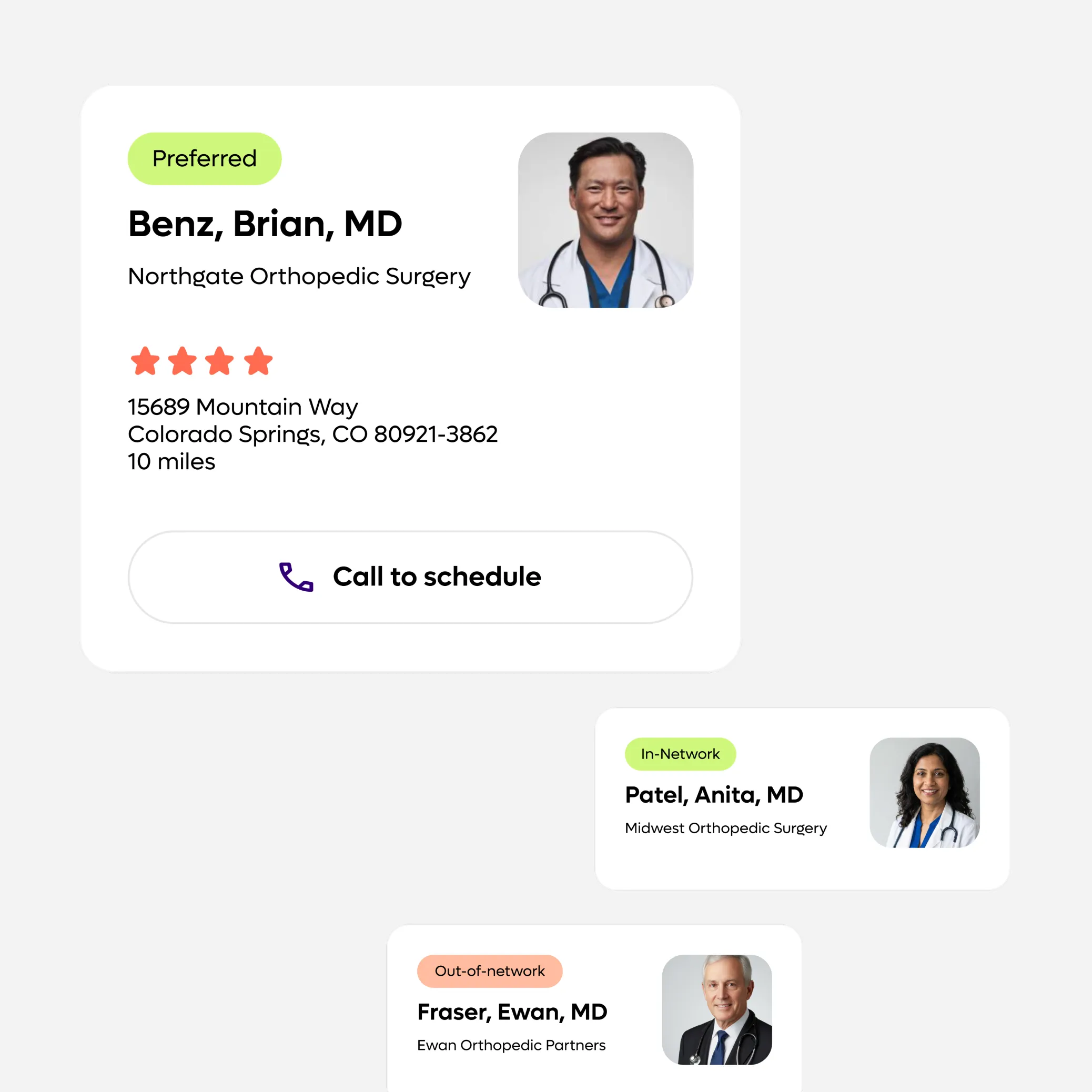
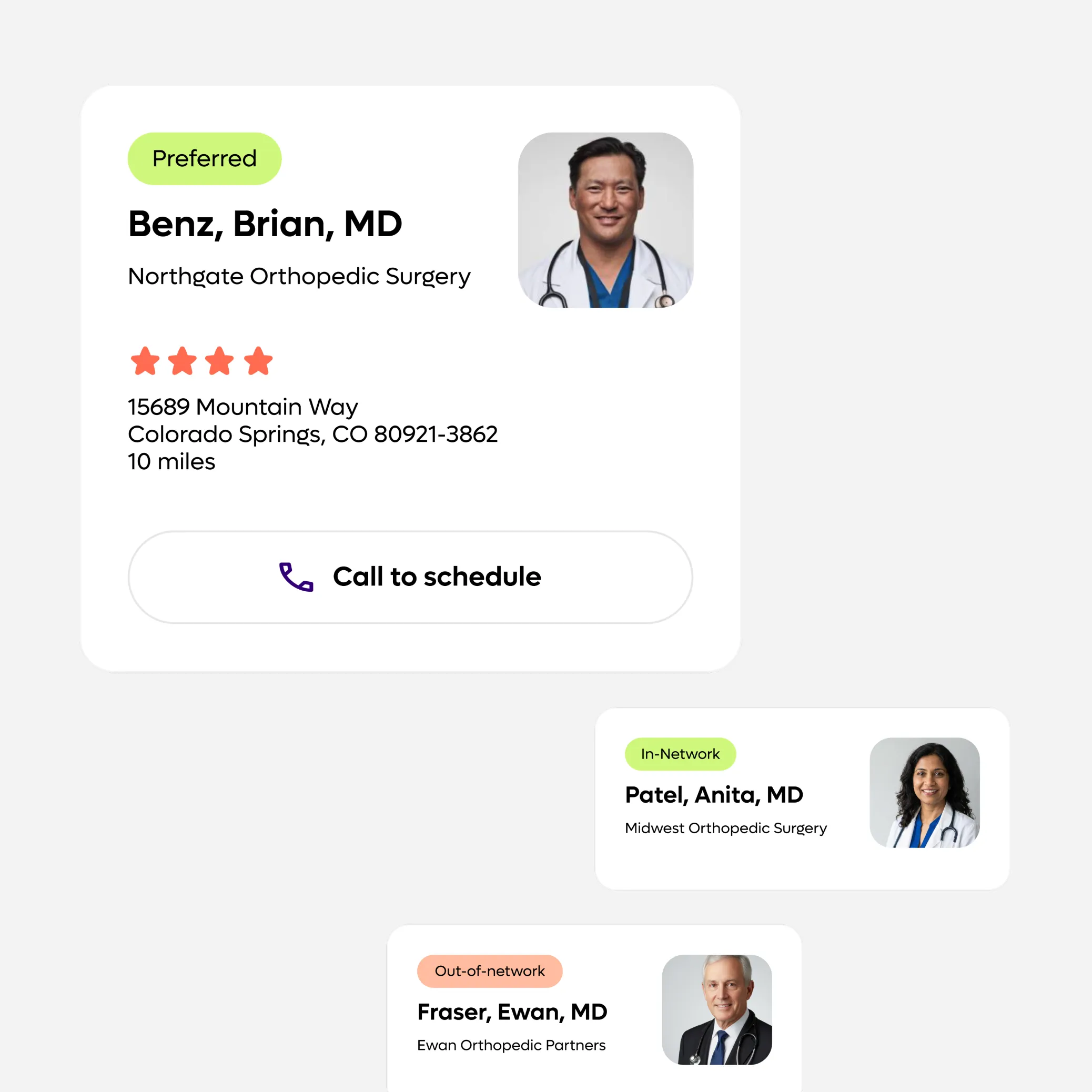
Precision Network Navigation
Integrate your preferred networks and tier structures directly into the provider search experience. Members are guided to the right providers with less friction, reducing noise, leakage and unnecessary out-of-network claims.
You power better benefits. We power you.
Learn more about Opyn’s solutions for TPAs:







