Connected journeys. Clear costs. Smarter member decisions.


Cut costs. Reduce friction. Protect retention.
- Lower cost to serve
- Fewer prior-auth andservice delays
- Clear, predictable cost and coverage answers
- Stronger employer and member retention
- Better operational consistency and compliance
Change Is Imminent, Are Health Plans Prepared for the Future?

Opyn features that power every touchpoint.
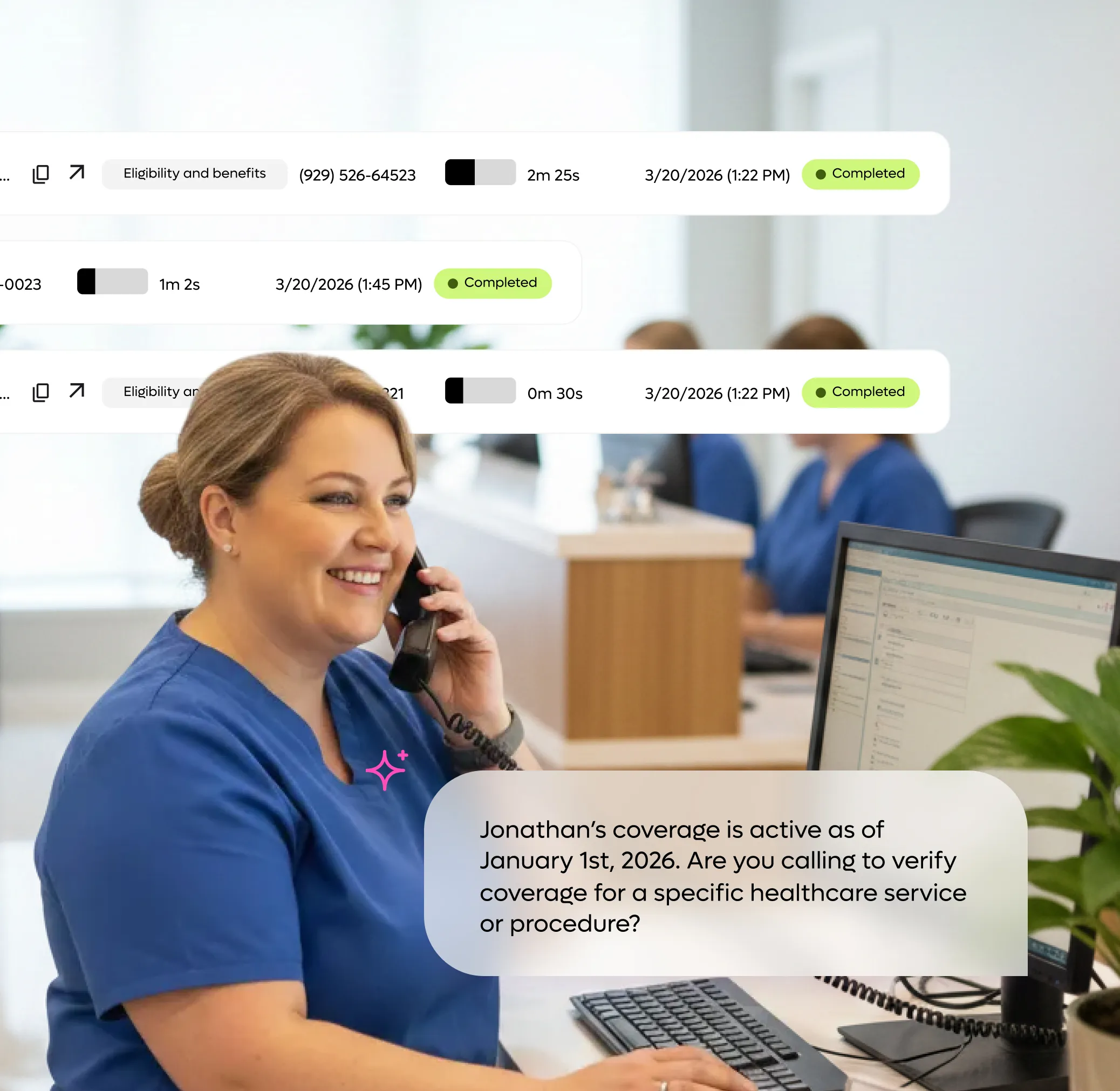
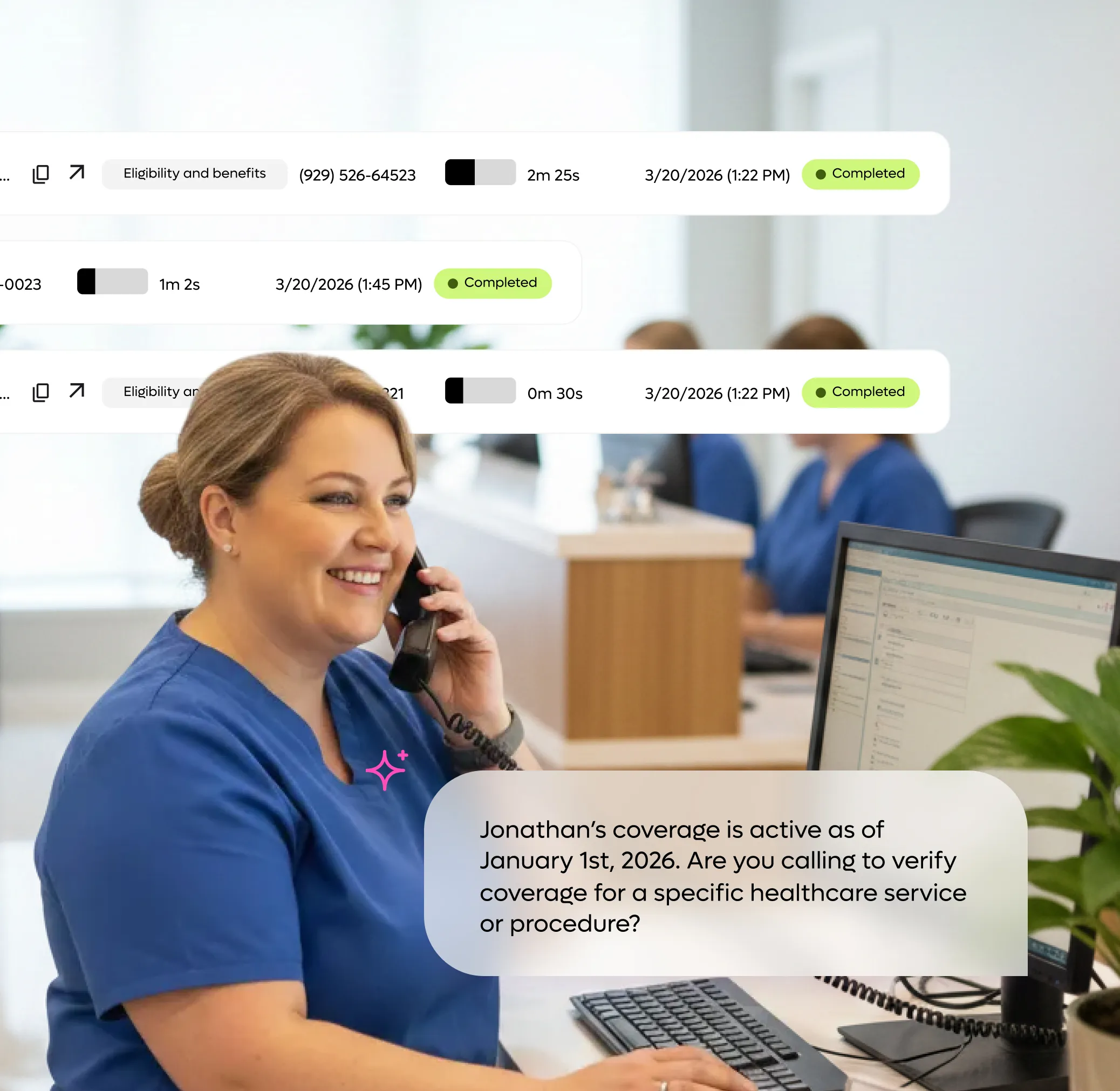
Automate the Front Line of Your Provider Relations
Don’t let routine inquiries slow down your plan’s operations. Our AI Agent provides your network with 24/7 self-service for their most frequent questions. By delivering instant, accurate answers without a phone call, you remove administrative hurdles and allow your team to focus on high-value clinical outcomes.
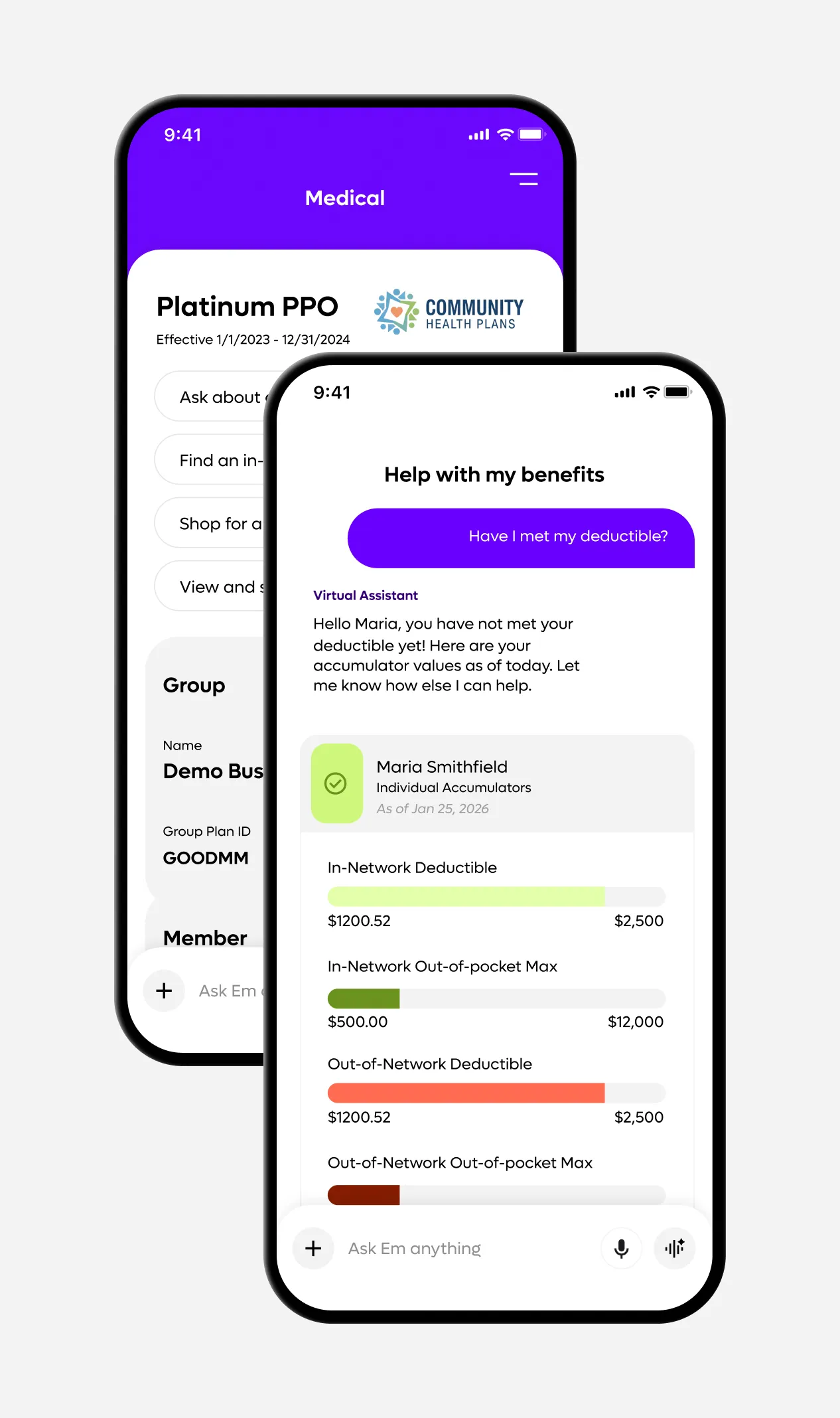
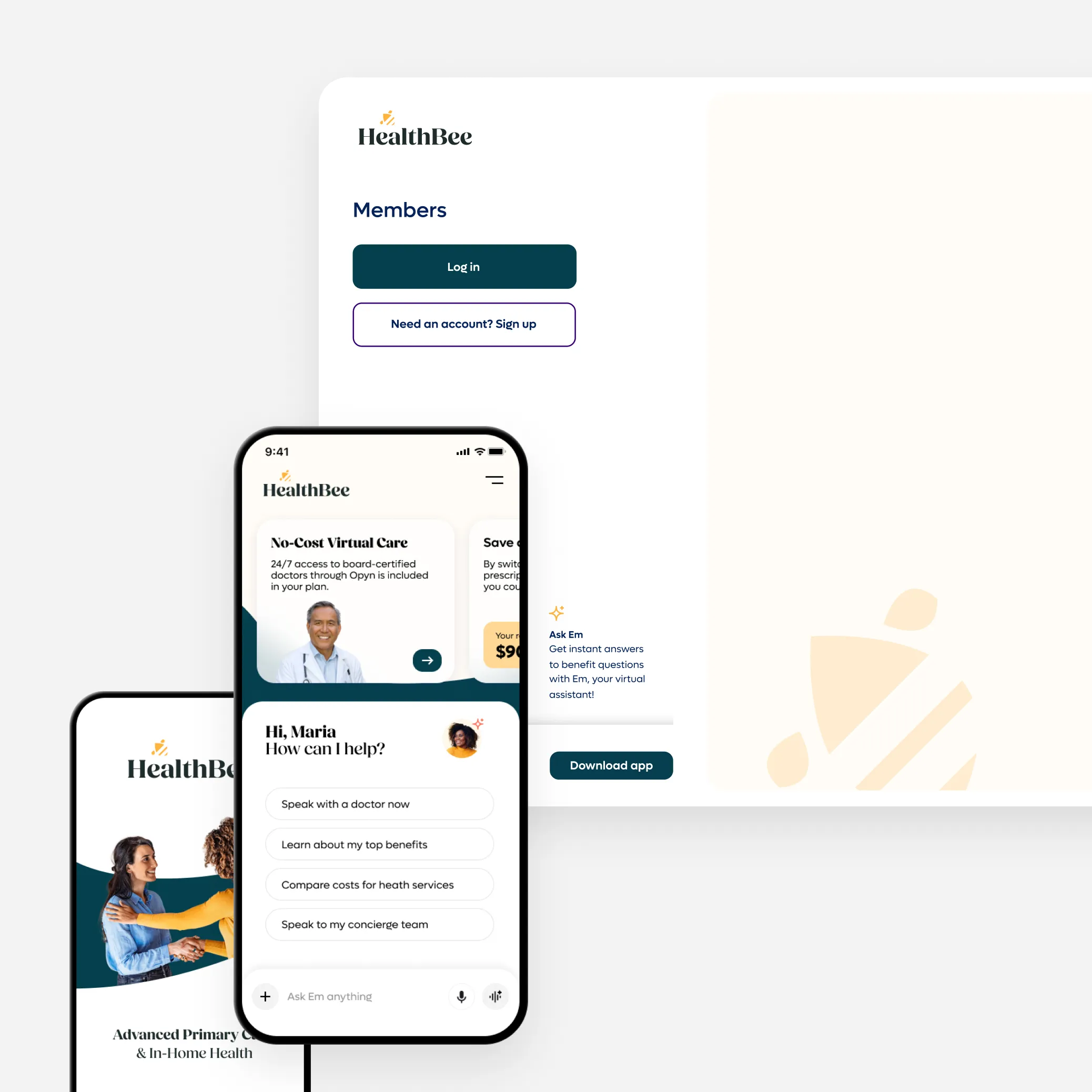
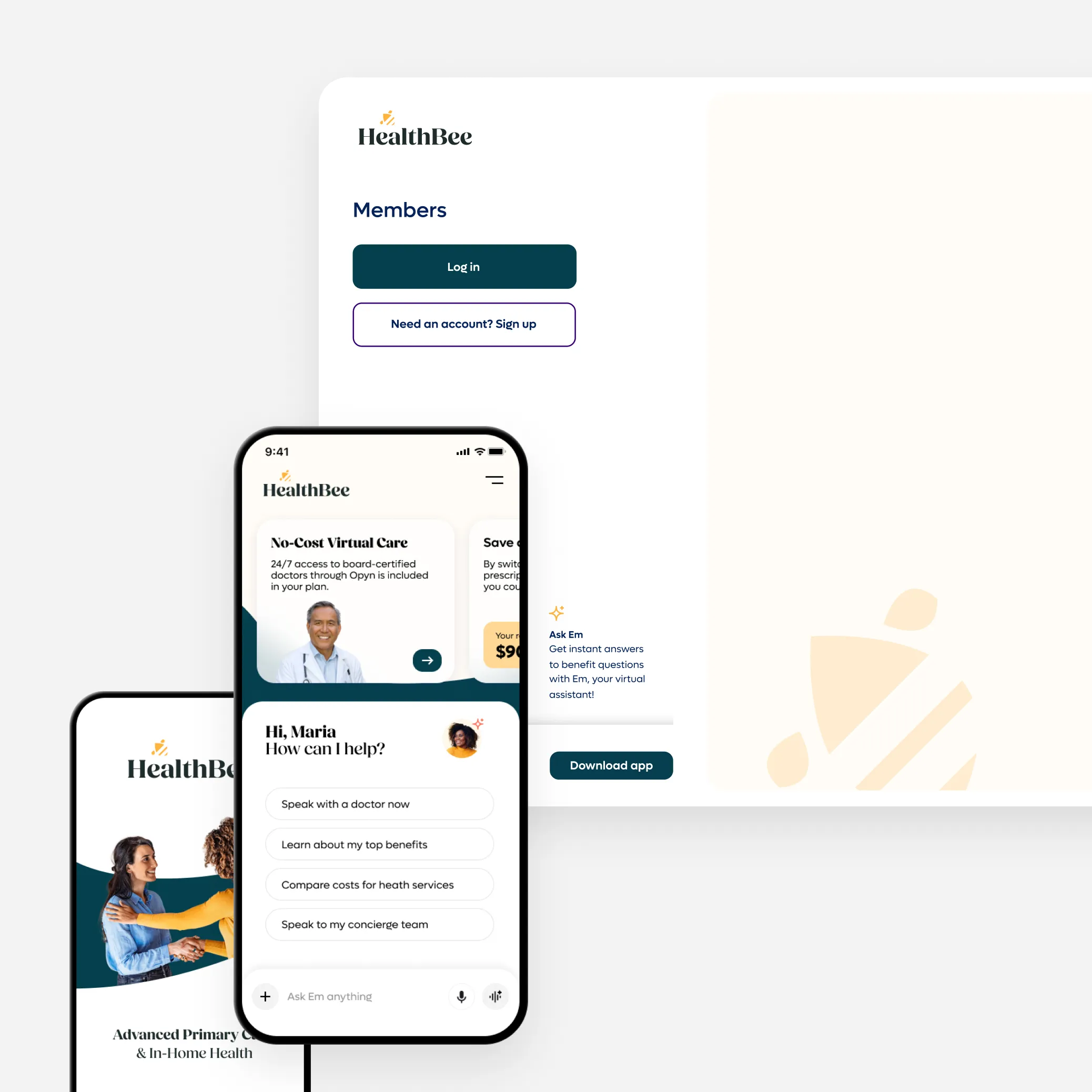
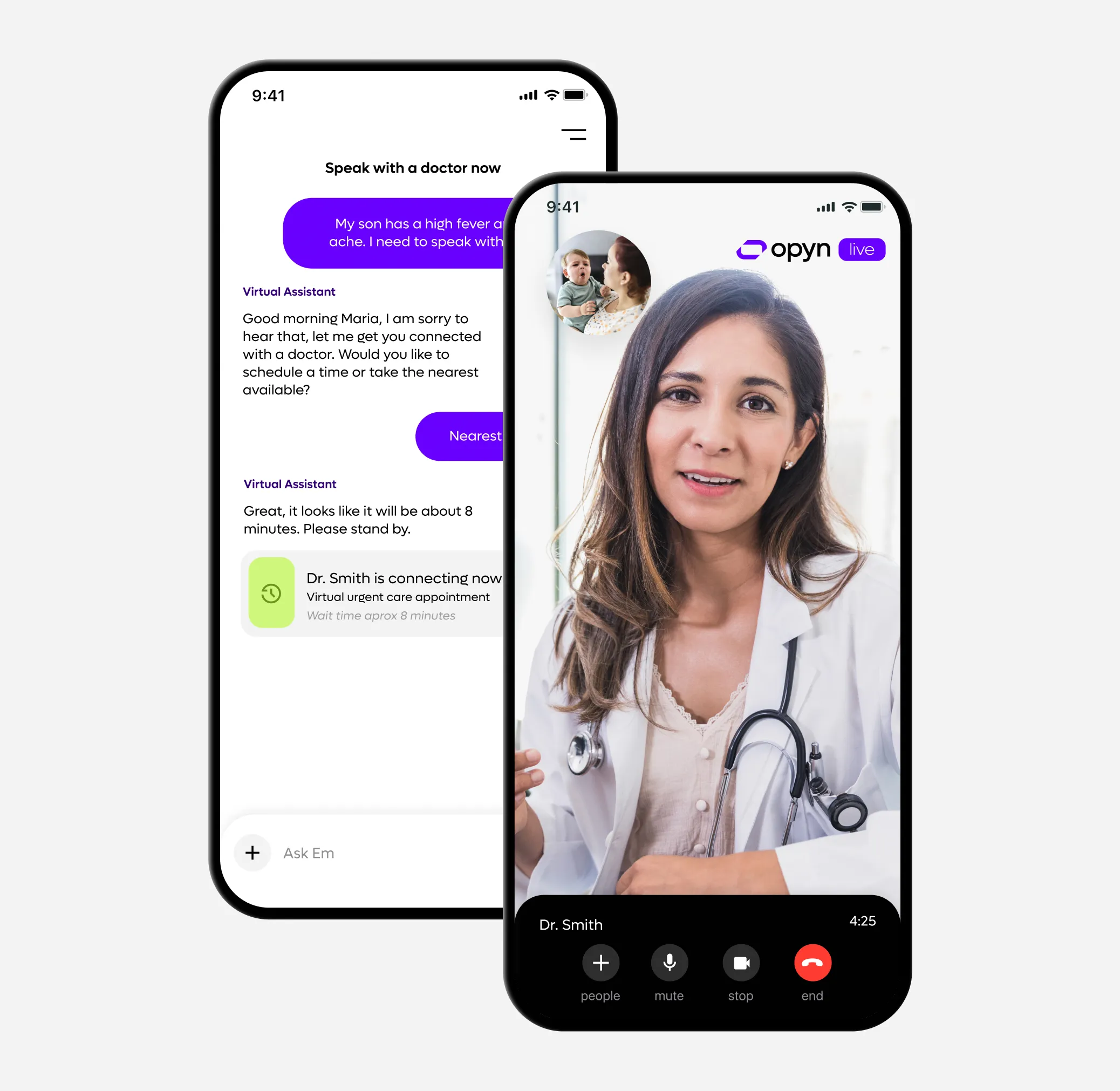
Own the Experience, AI the Navigation
Provide a unified, white-label platform that connects members, employers, and brokers under your brand. Our AI assistant helps members self-navigate their health plans in real-time, reducing your administrative load by turning complex back-office workflows into seamless, automated experiences.
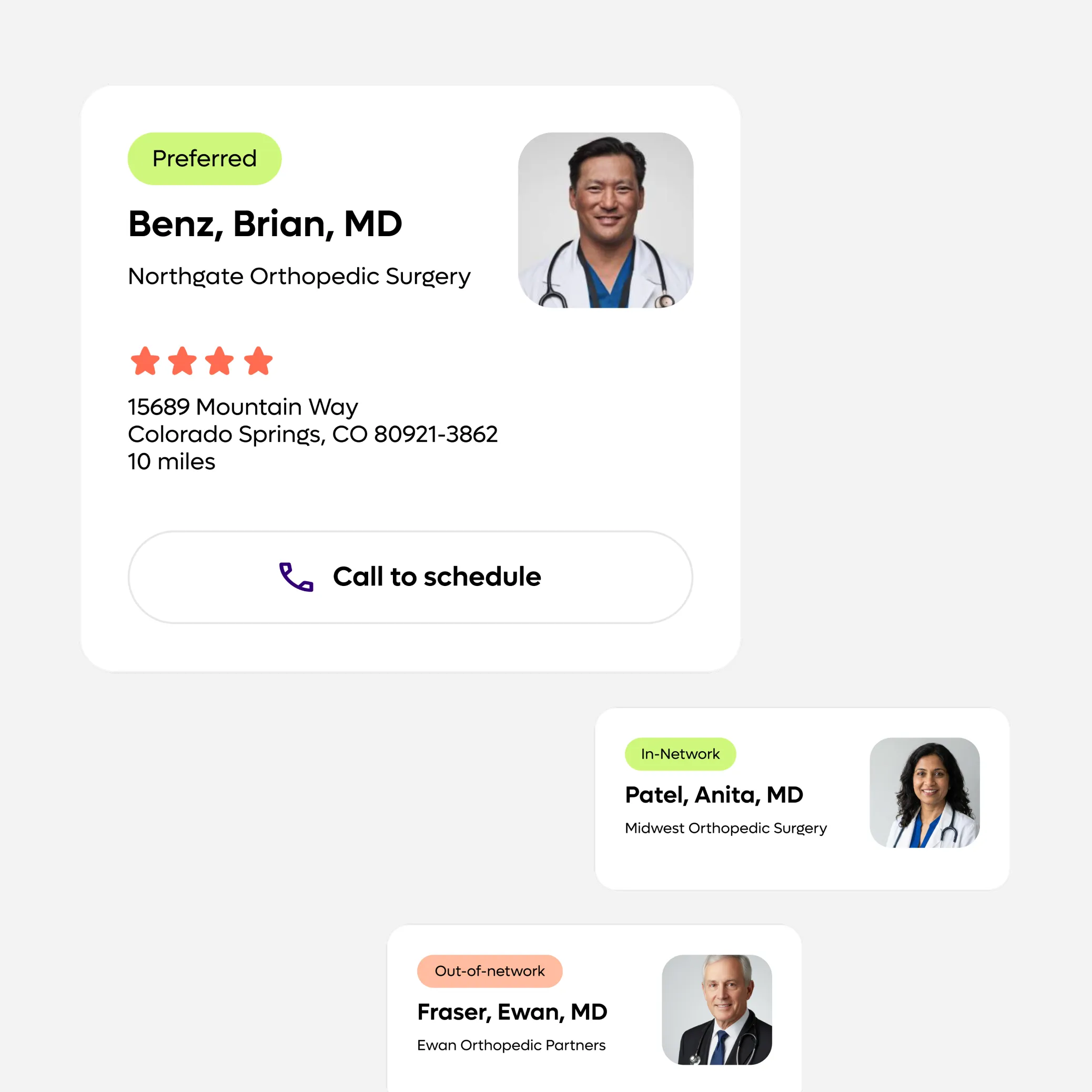
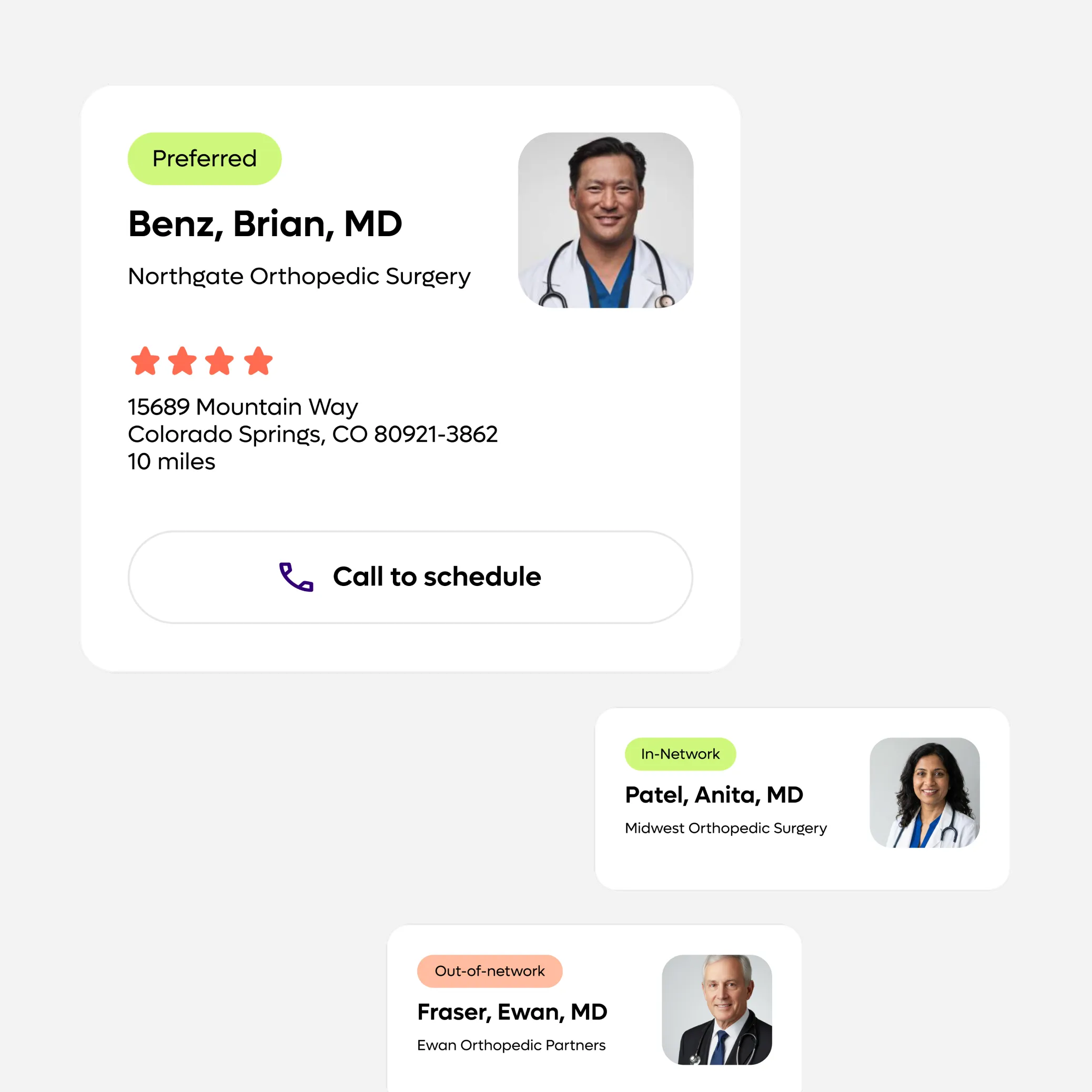
Compliance as a Competitive Edge
Turn transparency mandates into a member magnet. Our Transparency Solution powers intelligent provider search and care navigation—guiding members toward high-value, in-network options while reducing unnecessary spend.
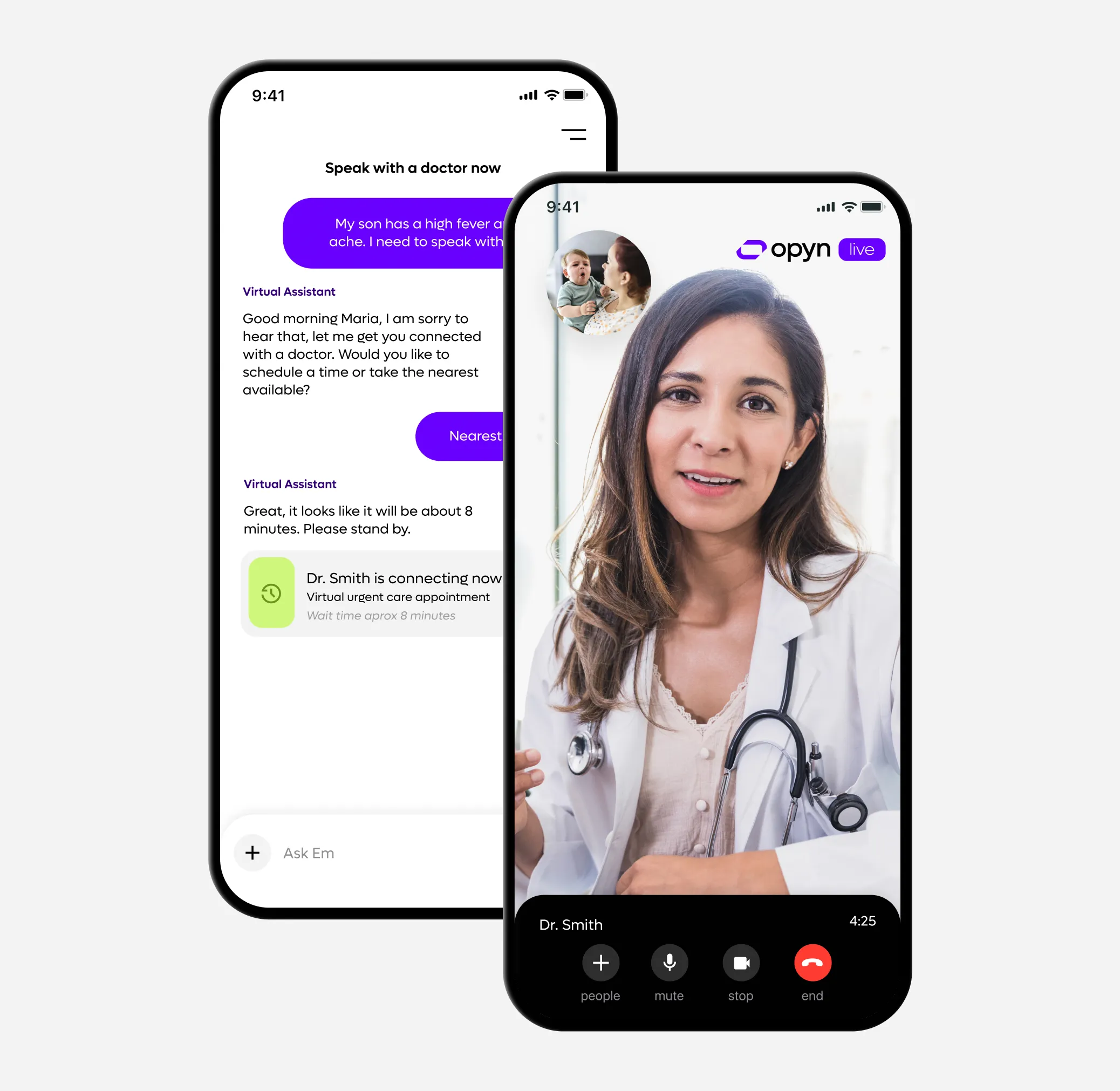
Fully Integrated Virtual Care
Offer a seamless, connected ecosystem. Members can review benefits, check costs, and access 24/7 virtual primary + behavioral care—all within the same interface.
You power better benefits. We power you.
Learn more about Opyn’s solutions for Health Plans:







